Until now, many pathogens still carry a high disease burden and remain elusive to prevention by means of vaccination. New approaches for the development of efficacious vaccines are one of the most pressing needs of our society. We have led an interview with Prof. Bruno Correia, tenure-track assistant Professor in Bioengineering at the EPFL, to discuss current challenges and understand perspectives in relation with vaccine development.

What is your work as a researcher in basic science in relation to vaccines development?
When we use the word vaccine, we should be very careful because vaccines can change the course of humanity so if you use that word, you must be prepared to deliver. A vaccine is not an experimental concept. It is something that works. For that reason, I consider our work still far from a real vaccine.
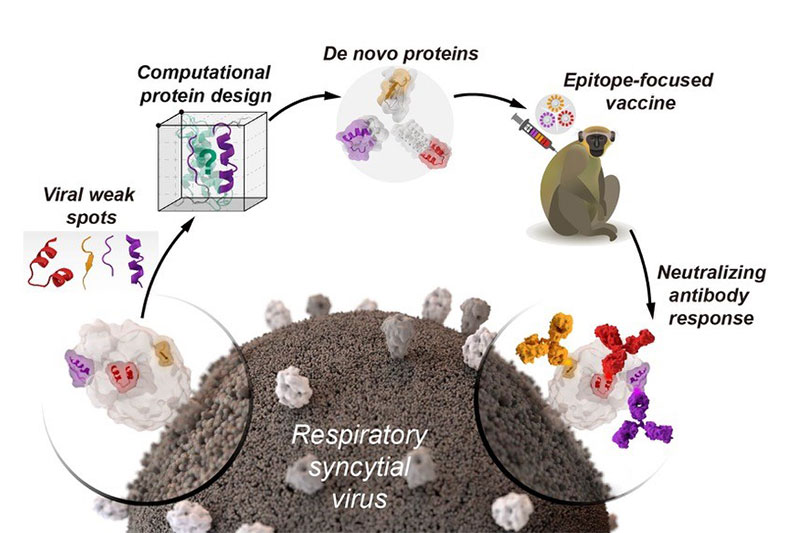
In my lab, what we have right now is a concept related to how we can use molecular engineering in order to control the behavior of antibody-based responses. How can we design proteins that can mimic these sites? How can we engineer them as best as possible? We use computational tools and a lot of experimental high-throughput screening to build around the idea of controlling the fine specificities elicited by the immune system that could potentially afford the highest possible levels of protection. We aim to produce protein-based vaccines driven by structural principles, in the long run. Because at some point, even the viral proteins that we use do not really work for influenza. They work for influenza for one season, but after that season, one is no longer protected. If we could elicit the right type of antibodies, perhaps we could solve this problem, this could also be interesting for HIV or dengue.
In the last years, we have taken some steps forward in trying to show how these molecular entities can be used to do that. I am still afraid of calling them a vaccine, because right now I don’t know if they are one, but at least we are exploring the potential with the preclinical models we have.
We know that vaccines are extremely important to prevent many diseases. What are the main limitations explaining why we don’t have vaccines for most of the infectious diseases?
Before going to the scientific problems, let’s not forget that there is also an economical component into all this. Academic institutions do not have the power, the means, or even the role, of developing mass production of vaccines or drugs for the widespread population. We can do basic research, we can develop preclinical concepts, etc., yet, from what we do to the point of bringing something into the society, there is a large gap which is generally covered by pharmaceutical companies. The latter are run by profit and that makes them sometimes take decisions that should be less influenced by the economic factors. It is sad to say, but perhaps if a vaccine had been further developed when the first SARS epidemic occurred, maybe today we would be in a different situation with the COVID-19 pandemic.
What about the scientific challenges related to vaccines?
We can start for example with RSV (Respiratory Syncytial Virus). The RSV vaccine has been pursued since the sixties. Until we could figure out how a vaccine like that could be made, it was tough! But right now, the scientific community has shown that presenting to the immune system a protein that is stabilized in a specific way may trigger more potent immune response. This is a great scientific achievement. Now it is time for the pharmaceutical industry to take this further and we’ll see if in the end, it’s going to be protective since there are lots of things we still don’t understand.
Let’s also talk about HIV. It is clearly one of these viruses that are very well endowed with strategies to escape the immune system. It just can do anything and everything. I would dare to say that most of the efforts that came out from HIV vaccine development are not true vaccines, but are mostly basic biology concepts at this point. I think we are far away from an HIV-vaccine, honestly, and this is really because HIV is particularly good at tricking the immune system.
Another vaccine that we could talk about is influenza. We have seasonal vaccines for influenza. One of the holy grails in the field is to have a universal influenza vaccine. However, with influenza it seems that the immune system builds up a memory of the first viruses that it sees and then it gets stuck in that immunological status. When the immune system encounters new viruses, it cannot mount a protective immune response. That, by itself, is not a vaccinology issue. It is a basic biology issue. We just don’t fully understand how the immune system works in that case. Through vaccinology, we are going to try to overcome that behavior of the immune system.
I could be here telling you how vaccines could potentially also be a way to avoid, for instance, the use of antibiotics. If we had better vaccines against bacterial pathogens, perhaps we would not need so many antibiotics. This is something that we, scientists, need to think about very seriously.
What are the advantages and disadvantages between using live-attenuated virus or using protein-based vaccines?
If you can use a live attenuated virus and it works, then this is what should be done. Especially if you have managed all safety issues and elicited the right type of protective immune response.
However, when live attenuated viruses do not work, what can we do? This is what happens for example with viruses such as HIV or RSV. Any kind of virological entity that replicates, seems to generate stronger immune response compared to anything we can produce with protein-based vaccines. However, it is a living organism and safety issues are always a problem. When they don’t work you need other solutions, and here is when protein-based vaccines seem to be the safest solution you can come up with.
The biggest problem with protein-based vaccines is that they often trigger very low immune responses. Nonetheless, there are a number of different strategies in terms of adjuvants and delivery of these antigens to enhance their immunogenicity.
Following your record of publications on that topic, we can see that one of the differences has been the methodological approaches you have been using. In 2010 the proteins you used were repurposed from nature and in 2014 you started designing proteins from scratch in the computer, that gave higher immunogenicity. What have you learnt during all those years working on that?
Yes, I think this is still the million-dollar question. We have learned a lot about protein engineering and we have developed a number of interesting tools to design proteins with a level of complexity that we could not have imagined ten years ago. During this entire journey, there were a few milestones along the way: the 2010’s milestone, then the 2011/2012, and then the 2014’s milestone.
The first two were designed to target HIV; these two immunogens have never done much in vivo. Maybe it is nothing related to the quality of the antigens, but it is just related to how hard it is to actually make these antibodies against HIV.
Then, we downgraded to a virus that is less sophisticated than HIV, which is RSV. In RSV, we have learned that in fact, the designed antigens could have in vivo activity but what we have also learned it that there are no silver bullets. The idea that you would present one single epitope to the immune system and you would get an amazing immune response that would neutralize everything, has been just wishful thinking.
Then, in our 2020 work, we tried to upgrade it a couple of steps. First, we realized that perhaps the immunological response to a single epitope was not good enough. For this reason, we tried to expose to the immune system three antigenic surfaces instead of only one, to give something more on what to work with. However, this also did not seem to be a silver bullet. Nonetheless, the activity seems to be better and more detectable than if you just present one (which I think is intuitive but from what is intuitive to what you actually observe, there is a big difference).
But then, I think that what was really interesting, was this idea of shaping and guiding the immune response. Once the immune system has been previously primed, could you focus the immune response to be effectively in specific sites that you want? This was a realization that we did not know, and again, it is intuitive that it would happen, but needed to be proved.
I think this could be an interesting application. Particularly for pathogens for which we have been exposed multiple times along our lifetimes (influenza, RSV, …) and now you just want to specifically bring up the functional response which can neutralize the pathogen. Because you don’t want to have nonfunctional antibodies around for a number of different reasons. Of course, I’m excited to push it further, both on the RSV, but also in influenza, again with the realistic perspective that a vaccine is something that changes the course of humanity and that the immunogens that we develop may not be something that will have that level of impact.
—
References:
- Computational Design of Epitope-Scaffolds Allows Induction of Antibodies Specific for a PoorlyImmunogenic HIV Vaccine Epitope, Structure, 2010.
- Proof of principle for epitope-focused vaccine design, Nature, 2014.
- Computation-Guided Backbone Grafting of a Discontinuous Motif onto a Protein Scaffold, Journal of Molecular Biology, 2011.
- De novo protein design enables the precise induction of RSV-neutralizing antibodies, Science, 2020.

Leave a comment
The editors reserve the right not to publish comments or to abridge them.